What is HPV?
HPV stands for Human Papillomavirus and consists of more than 200 related viruses, some spread through vaginal, anal, or oral sex. There are two groups of HPV – non-oncogenic or low-risk HPV, which causes warts, and oncogenic or high-risk HPV, which causes cancer. There are approximately 14 high-risk or oncogenic HPV types that can cause several types of cancer. They include HPV 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 66, and 68, but HPV 16 and HPV 18 are responsible for most HPV-related cancers.
HPV infection is incredibly common in teens and adults in the United States. Most of the time, your immune system will get rid of an HPV infection by itself within two years, regardless of which type you have, but there is still a possibility that high-risk HPV will progress into cancer.
Most people who have HPV don’t know because there are rarely symptoms associated with infection. This makes HPV very easy to pass to others without realizing it. HPV is passed through skin-to-skin contact, particularly through sexual activity.
What are HPV-Associated Cancers?
If your immune system can’t get rid of an oncogenic HPV infection, over time your normal cells will become abnormal or precancerous. If those abnormal cells aren’t caught and removed in time, they can develop into cancer. The cancers associated with HPV infection include cervical, vaginal, vulvar, penile, anal, and certain head and neck (oropharyngeal) cancers.
Who do HPV-Associated Cancers Affect?
Anyone who is sexually active and unvaccinated can contract HPV, which can then turn in to an HPV-associated cancer over time. Keep scrolling to learn about risk factors for each type of HPV-associated cancer.
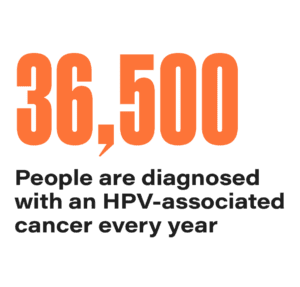
Facts About HPV-Associated Cancers
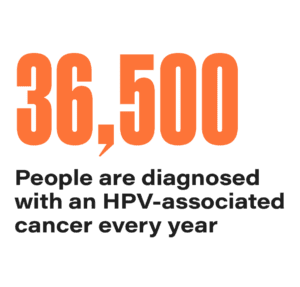
HPV is responsible for more than,
60-70% of head and neck cancers
90% of anal and cervical cancers
70% of vaginal and vulvar cancers
60% of penile cancers
*Note: These statistics are based on the U.S. population.
Risk Factors for HPV-Associated Cancers
Risk factors for HPV-associated cancers can either be genetic or based on your lifestyle. Whether you have just one of these risk factors or all of them, there is no guarantee you will develop cancer in your lifetime. But risk factors are important to understand so you can adjust any lifestyle-based risks, talk to your doctor about your overall risk, and develop an appropriate screening plan to catch cancer early if it does develop.
If You Were Assigned Female at Birth
- Being older than 30
- Having a long-term infection with certain types of HPV
- Having several sexual partners or having a partner who has previously had many sexual partners themselves
- Starting to have sex at a young age
- Having receptive anal sex
- Using tobacco products including cigarettes, pipes, cigars, and chewing tobacco
- Drinking alcohol
- Using birth control pills for 5+ years (but this risk gradually declines after stopping)
- Giving birth 3+ times
- Your mother taking Diethylstilbestrol (DES), a hormone drug that was used from 1940-1971 to prevent miscarriage, while pregnant with you
- Being immunocompromised due to HIV or another condition
- Being diagnosed with vaginal adenosis
- Being diagnosed with vulvar intraepithelial neoplasia (VIN)
- Being diagnosed with lichen sclerosus
- Being diagnosed with anal warts
- Having an inherited genetic mutation like Fanconi Anemia or Dyskeratosis Congenita
- Having had cervical cancer or pre-cancer, vaginal cancer, or vulvar cancer
- Having a personal or family history of melanoma or atypical moles
- Being overweight or obese
- Being exposed to UV light (aka sunlight) for long periods of time
- Eating a diet low in fruits and vegetables
If You Were Assigned Male at Birth
- Being older than 55
- Having a long-term infection with certain types of HPV
- Having multiple sex partners
- Having receptive anal sex
- Not being circumcised
- Using tobacco products including cigarettes, pipes, cigars, and chewing tobacco
- Drinking alcohol
- Undergoing UV light treatment of psoriasis (PUVA therapy)
- Being immunocompromised due to HIV/AIDS or another condition
- Having phimosis
- Having anal warts
- Having an inherited genetic mutation like Fanconi Anemia or Dyskeratosis Congenita
- Being overweight or obese
- Being exposed to UV light (aka sunlight) for long periods of time
- Eating a diet low in fruits and vegetables
HPV-Associated Cancers Warning Signs
Cervical Cancer Warning Signs
- Vaginal bleeding that starts and stops between your regular menstrual period
- Vaginal bleeding that causes your period to last longer than normal or be heavier than normal
- Vaginal bleeding after sexual intercourse, douching, a pelvic exam, or menopause
- Increased vaginal discharge
Vaginal Cancer Warning Signs
- Abnormal vaginal bleeding (often after sex) or vaginal discharge
- A mass or lump in the vagina that can be felt
- Pain during sex
- Painful urination
- Constipation
- Pain in the pelvis, low in the belly, or the back
- Swelling in the legs
Vulvar Cancer Warning Signs
- Itching, pain, or burning that does not go away or get better
- An area of your vulvar skin that looks different from the rest, including being thicker, lighter or darker, or red or pink
- A bump, lump, or open sore
- Bleeding or discharge not related to your normal menstrual period
Penile Cancer Warning Signs
- A change in the skin of the penis, including the skin getting thicker or changing color, a new lump or ulcer, a rash under the foreskin, small and crusty bumps, flat bluish-brown growths, or smelly discharge or bleeding under the foreskin
- Swelling at the end of the penis
- Lumps under the skin in the groin area
Anal Cancer Warning Signs
- Bleeding from the rectum
- Itching in or around the rectum
- A lump or mass at the anal opening
- Pain or a feeling of fullness in the anal area
- Narrowing of stool or other changes in bowel movements
- Abnormal discharge from the anus
- Incontinence (loss of bowel control)
- Swollen lymph nodes in the anal or groin areas
Head and Neck (Oropharyngeal) Cancer Warning Signs
- Pain or a sore on the lip or in the mouth that doesn’t heal
- A lump in the lips, mouth, cheek, neck, or back of the throat
- A white or red patch on the gums, tongue, tonsil, or lining of the mouth
- A long-lasting sore throat or feeling that something is caught in your throat
- Trouble chewing, swallowing, or moving the jaw or tongue
- Numbness of the tongue, lip, or other part of the mouth
- Swelling or pain in the jaw
- Loosening of the teeth or pain around the teeth
- Voice changes
- Unexplained weight loss
- Earaches
Learn more about cancer Early Detection.
Notice a warning sign? Talk to your doctor, do not WebMD!
Preventing HPV-Associated Cancers
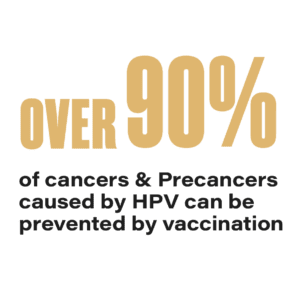
Get the HPV Vaccine
Over 90% of cancers and precancers caused by HPV can be prevented by vaccination. The HPV vaccine works best if you get it before you’ve been exposed to HPV. That’s why we recommend everyone ages 9-14 get the HPV vaccine on the suggested schedule, and anyone 15-26 who hasn’t been vaccinated yet should also get the HPV vaccine to catch up. Over 15 years of monitoring and research have shown that HPV vaccination is safe and effective.
Who Should Get the HPV Vaccine?
- Everyone 9-14 Years Old – Getting vaccinated against HPV between 9 and 14 years old is the best way to ensure you are protected against the virus before you can be exposed. You’ll need to get 2 doses (shots) to complete the vaccine series, which are given 6-12 months apart. Getting vaccinated in this age group can prevent more than 90% of HPV cancers throughout your lifetime.
- Everyone 15-26 Years Old – If you haven’t been vaccinated against HPV yet, you can and should still get the vaccine up to age 26. You may have been exposed to some types of HPV prior to vaccination, but the vaccine can still protect you against the other types you haven’t yet encountered. If you get vaccinated after age 15, you’ll need to get 3 doses (shots) to complete the vaccine series, which are given over 6 months.
- Everyone 27-45 Years Old – Talk to your doctor about if the vaccine is right for you if you haven’t yet been vaccinated.
The HPV vaccine is covered by most insurance plans. If your child doesn’t have insurance, the Vaccines for Children (VFC) program will cover the cost of the HPV vaccine. No matter what, the HPV vaccine should be free for you to get.
Practice Safe Sex
It’s important to practice safe sex to lower your chance of contracting a sexually transmitted infections (like HPV) that can, over time, increase your likelihood of developing cancer. This includes consistently and correctly using condoms and/or dental dams, limiting the number of sex partners you have, and avoiding sex with people who have had many other partners themselves. Even if you’ve gotten the HPV vaccine, it’s important to practice safe sex to protect yourself against other STIs.
Learn more about cancer Prevention.
Finding HPV-Associated Cancers Early
Unfortunately, the only HPV-associated cancer that can be found early through screening is cervical cancer. Cervical cancer early detection includes routine Pap tests and/or HPV tests. Starting at 21 years old, you should talk to your doctor about when to start screening based on your risk factors and family history of cancer, and at 30 years old you should start getting a Pap test and/or HPV test every 3-5 years. Visit our cervical cancer page to learn more.
Treatment Options for HPV-Associated Cancers
There is no available treatment for HPV itself, but the cell changes that HPV causes, such as precancers and genital warts, can be treated. There are different treatment approaches for each of the individual HPV-associated cancer types.
To learn more about what to expect at your first treatment appointment, visit our Life With Cancer page.
After Treatment for HPV-Associated Cancers
After finishing treatment for an HPV-associated cancer, there is always a chance of recurrence, where your HPV-associated cancer can come back, or a second cancer, where you are diagnosed later in life with an additional type of cancer. Making healthy lifestyle choices can help prevent a second cancer from developing.
Common Experiences of People with HPV-Associated Cancers
Cancer is unique and each person’s experience is completely valid. But some feelings can be universal. Here are a few common, but less discussed, experiences you might have with an HPV-associated cancer diagnosis:
Thinking That Cancer is Your Fault Because You Have HPV
Spoiler Alert: cancer is never your fault. Just because you have HPV doesn’t mean you caused your cancer. In fact, most HPV infections don’t cause cancer and cancer can affect anyone.
Feeling Embarrassed to Talk About Your Cancer
Because most of the HPV-associated cancers have to do with your sex organs, it can feel awkward or embarrassing to say that you’ve been diagnosed with that type of cancer. If you’re feeling this way, just remember that your doctor and treatment team will never be embarrassed to discuss your cancer with you.
Source: American Cancer Society; Centers for Disease Control and Prevention