What is Lung Cancer?
Lung cancer is a type of cancer that starts in your lungs. There are two main types of lung cancer.
Non-Small Cell Lung Cancer
Approximately 87% of all lung cancers are non-small cell lung cancers, which is an umbrella term for several types of cancer, including adenocarcinomas, squamous cell carcinomas, and large cell carcinomas.
Small Cell Lung Cancer
Small cell lung cancers account for ~13% of all lung cancers, are found almost exclusively in heavy smokers, and tend to grow and spread faster than Non-Small Cell Lung Cancers.
Who Does Lung Cancer Affect?
Lung cancer mostly occurs in people who are older than 65 years old. If you are a cigarette smoker, or have been in the past, you are at greater risk for lung cancer. But lung cancer can affect anyone, whether you’re a smoker or not.
In 2025,
226,650 new diagnoses
124,730 people will die
During their lifetime,
1 in 17 women will be diagnosed
1 in 16 men will be diagnosed
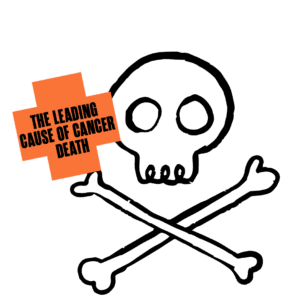
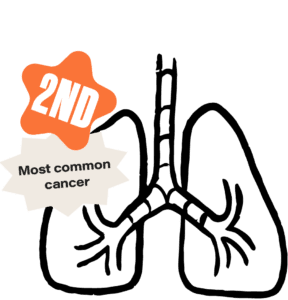
Lung Cancer Facts
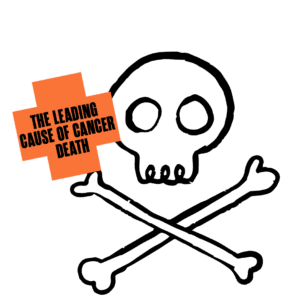
Lung cancer has a
27% 5-year survival rate
Black men are approximately 12% more likely to be diagnosed with lung cancer than white men. Black women are approximately 16% less likely to be diagnosed with lung cancer than white women. Black, Latino, Asian, Pacific Islander, and American Indian/Alaska Native people are all less likely than white people to be diagnosed with lung cancer early when it is easier to treat. Only Asians and Pacific Islanders are more likely to survive five years after a lung cancer diagnosis compared to white people. Black (21% less likely), Latino (16% less likely), and American Indian/Alaska Native (13% less likely) people are all less likely to survive five years after diagnosis compared to white people. Additionally, people who live in rural areas have substantially higher lung cancer incidence rates than people who live in more urban places.
*Note: All statistics are based on the U.S. population.
Why? For the most part, differences in cigarette smoking habits explain lung cancer incidence rates among different races and genders in the U.S.
Why? Increased mortality among Black, Latino, and American Indian/Alaska Native people may be due to lower cancer screening rates, which results in later diagnosis and decreased access to the most effective types of treatment.
Why? American Indian/Alaska Native women and people who live in rural areas tend to live further away from cancer care, making their cancer more challenging to treat.
Lung Cancer Risk Factors
The risk factors of lung cancer are a combination of your genetics and lifestyle choices. Whether you have one or all of these risk factors, there is no guarantee you will develop lung cancer in your lifetime. Risk factors are important to understand so you can adjust your lifestyle-based risks and talk to your doctor about your overall risk.
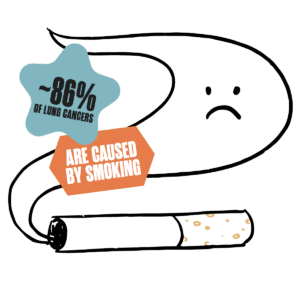
- Tobacco smoke, including smoking cigarettes, cigars, pipes, low-tar or “light” cigarettes, and menthol cigarettes, and risk increases with quantity and duration of smoking.
- What about weed and vaping? There’s still more research needed to fully understand the impact of weed and vaping on cancer. But, smoking anything isn’t good for you, especially if you smoke a lot. Try alternative ways of getting a THC and/or CBD high, such as edible or topical products.
- Secondhand smoke
- Radon gas exposure, which is found in homes and other buildings in the U.S.
- Working with asbestos, such as in mines, mills, textile plants, places where insulation is used, and shipyards
- Other carcinogen exposure, including arsenic, chromium, cadmium, and diesel exhaust
- Previous radiation therapy to the lungs
- Air pollution
- Personal or family history of lung cancer
- Working in rubber manufacturing, paving, roofing, painting, or chimney sweeping
Lung Cancer Warning Signs
Most people with lung cancer don’t experience any signs or symptoms until the cancer has spread. But, if you notice any of these symptoms, talk to a doctor:
- A cough that doesn’t go away or gets worse
- Coughing up blood or rust-colored phlegm, even a small amount
- Shortness of breath
- Chest pain that is more extreme with deep breathing, coughing, or laughing
- A hoarse voice
- Recurrent pneumonia or bronchitis
- New wheezing
- Loss of appetite
- Unexplained weight loss
- Feeling tired or weak
Learn more about cancer Early Detection.
Notice a warning sign? Talk to your doctor, not WebMD!
Preventing Lung Cancer
While lung cancer can’t exactly be prevented, you can lower your risk of lung cancer by making healthy lifestyle choices, including not smoking, avoiding secondhand smoke exposure, and reducing your exposure to other carcinogens like radon.
Learn more about cancer Prevention.
Finding Lung Cancer Early
We say it all the time: Early detection saves lives. By finding lung cancer early, it is easier to treat and there are better treatment outcomes.
Low-Dose CT Scan
This screening takes x-ray images of your lungs to look for abnormal areas that could indicate cancer. Low-Dose CT Scans should be completed annually.
Who Should Get Screened?
If you are 50-80 years old with a 20+ pack-year smoking history and currently smoke or used to smoke, you should be screened for lung cancer every year.
Calculating Your Pack Year History
To know if you’re eligible for a Low-Dose CT Scan to find lung cancer early, you need to calculate your pack year history. Use this formula to figure it out.
Packs of cigarettes smoked per day
x Number of years you smoked
= Pack year history
If your pack year history is 20 or higher, you should talk to a doctor about getting a Low-Dose CT Scan to check for lung cancer.
Lung Cancer Treatment Options
Lung cancer treatment is personalized and depends on many factors, including the type of lung cancer you have been diagnosed with.
Treating Non-Small Cell Lung Cancer
- Surgery – Surgery is a common treatment option for early-stage non-small cell lung cancer. Depending on size and location of the tumor and how well your lungs are functioning, either a section of your lung or an entire lung will be removed during surgery.
- Chemotherapy – Chemo uses anti-cancer drugs injected into your body or taken orally to fight lung cancer. With lung cancer, chemo can be used before surgery to shrink the tumor size, after surgery to address any remaining cancer cells, or as a main treatment.
- Radiation Therapy – Radiation uses high-energy rays or particles to kill cancer cells and could include External Beam Radiation, where radiation beams are focused on the lungs from a machine outside of the body, and Brachytherapy, where small radioactive pellets (aka seeds) are placed into your airway to shrink tumors.
- Immunotherapy – Immunotherapy uses medicine to train your immune system to better recognize and destroy cancer cells.
Treating Small Cell Lung Cancer
- Chemotherapy – Chemo uses anti-cancer drugs injected into your body or taken orally to fight lung cancer. Chemo is typically used as a treatment for small cell lung cancer, and often given in combination with radiation and/or immunotherapy as well.
- Immunotherapy – Immunotherapy uses medicine to train your immune system to better recognize and destroy cancer cells.
- Radiation Therapy – Radiation uses high-energy rays to kill cancer cells by pointing a machine outside of your body at cancer cells within your body. For small cell lung cancer, radiation is typically used to treat the tumor and lymph nodes in your chest, after chemo is completed, to decrease the chances of the cancer spreading to your brain, to shrink tumors to relieve symptoms.
To learn more about what to expect at your first treatment appointment, visit our Life With Cancer page.
After Lung Cancer Treatment
After finishing treatment, there is always a chance of recurrence, where your lung cancer can come back, or a second cancer, where you are diagnosed later in life with an additional type of cancer. Making healthy lifestyle choices can help prevent a second cancer from developing.
Common Experiences of People with Lung Cancer
While each person’s experience with lung cancer is personal and unique, there are some common experiences that people with lung cancer may be going through.
Thinking Lung Cancer is Your Fault Because You Smoke
Spoiler Alert: cancer is never your fault. Just because you currently or used to smoke doesn’t mean you caused lung cancer. While smoking does increase your risk of lung cancer, there are plenty of people who have never smoked a day in their lives and still get lung cancer. So stop beating up on yourself.
Feeling Like Everyone and No One Gets It, All At the Same Time
Lung cancer is common, but that doesn’t mean everyone who has experienced lung cancer has the same experience as you. It can be helpful to talk to people who’ve also been through this diagnosis, but your experience will also always be uniquely yours. Sometimes this dichotomy can feel confusing or frustrating.
Feeling Confused About Your Diagnosis
Most people have a picture in their mind of what someone who is diagnosed with lung cancer looks like, and maybe that’s just not you. If you’re not a smoker, are young, or don’t fit any of the other assumptions about people with lung cancer, it can feel confusing that this is the cancer you’ve been diagnosed with.
Source: American Cancer Society; Centers for Disease Control and Prevention; National Cancer Institute